July 17, 2023 – Singer-songwriter Lisa Marie Presley died from a “strangulated,” or twisted, small bowel on Jan.12, surprising many fans who had seen her attend the Golden Globe awards ceremony just days before. The daughter of the late Elvis Presley was 54 years old.
The Los Angeles medical examiner ruled Presley died of natural causes and, in a report issued last week, linked her small bowel obstruction to bariatric surgery she had years earlier. CNN, which first obtained the autopsy, said it included the official opinion of deputy medical examiner Juan M. Carrillo, MD, who said the obstruction was caused by “adhesions (or, scar tissue) that developed after bariatric surgery years ago. This is a known long-term complication of this type of surgery.”
Surgery experts don’t dispute that a cutoff of blood supply to her small bowel, also known as the small intestine, led to her death. But they’re less certain that internal scarring from previous weight loss surgery is to blame.
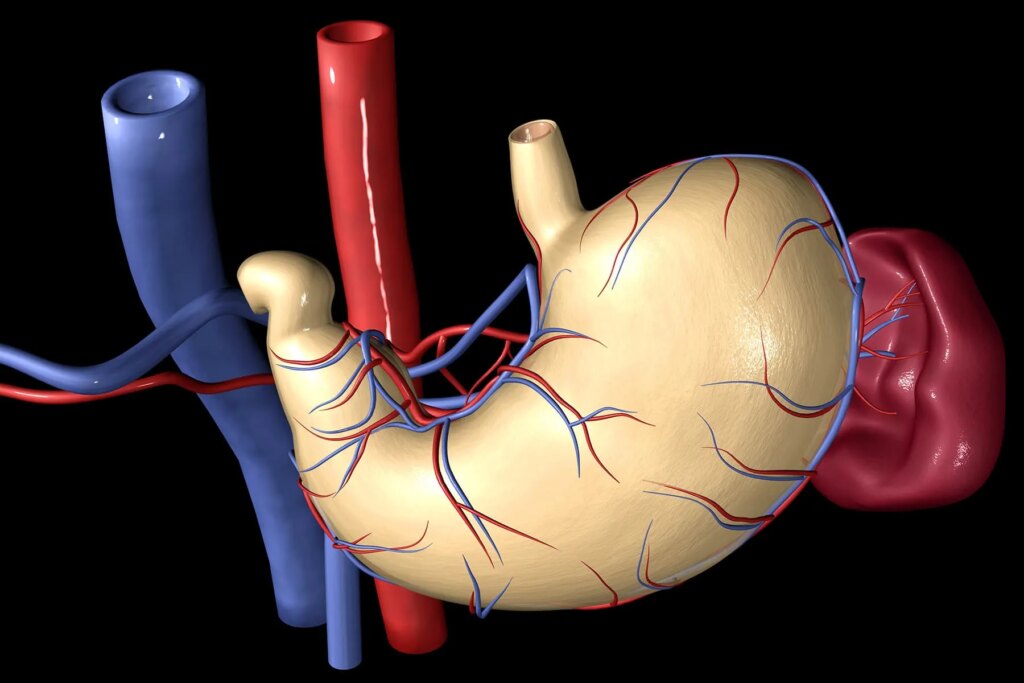
“It just doesn’t make exact sense to all of us [surgeons],” said Marina Kurian, MD, president of the American Society for Metabolic and Bariatric Surgery. “It sounds like she had a bowel obstruction for sure. But it’s not clear to me … that it is related to the bariatric surgery, because those scars would be right up by the liver and the stomach, and the small intestine is not usually up there.”
Presley reported belly pain earlier that day, according to the medical examiner. It’s unclear if her pain had persisted for days or come and gone in severe bouts, which are common signs of bowel obstruction. Vomiting and abdominal distention – when air or fluid gathers in the belly and causes it to expand – are also common.
In many cases, bowel obstructions can be treated if medical care is sought early enough. “The message is obviously if you have abdominal pain, and it’s persistent abdominal pain, go see a physician,” Kurian said.
Not All Bariatric Procedures are the Same
Bariatric surgery includes many different procedures, and Kurian thinks from the medical examiner’s report that Presley most likely had a single anastomosis duodenal ileostomy (SADI). This kind of procedure lowers food intake by reducing the stomach size and limits absorption of food by bypassing part of the small intestine.
A bowel obstruction can occur after many types of surgery, not just bariatric procedures. Gynecologic surgery, urinary system surgery, and general abdominal surgeries can leave internal scarring that causes this complication, said Kurian. “So it could very well have been from some other surgery.”
If left untreated, bowel obstructions can cut off blood supply, “which is unfortunately what happened in Ms. Presley’s case,” said Stacy Brethauer, MD, a bariatric surgeon and a professor in the Division of General and Gastrointestinal Surgery at Ohio State University Wexner Medical Center.
Nearly all bariatric procedures in the last two decades have been performed with minimally invasive techniques, like laparoscopy, that cause less scarring than open surgery, Brethauer said.
“Fortunately, bowel obstructions are quite rare now after laparoscopic bariatric surgery and occur in only 1-2% of patients long-term,” he said.
Short- and Long-Term Risks
Overall, the risks of bad outcomes after weight loss surgery are “very, very low,” Kurian said. Short-term risks include leaks, bleeding, infection, and blood clots. Long-term adverse effects can include bowel obstruction and malnutrition. The risk of malnutrition from lower absorption of nutrients can be lessened by patients taking multivitamins, for example.
For the vast majority of patients seeking bariatric surgery, the benefits far outweigh the risks, both in the short term and long term, Brethauer said. Benefits include significant reduction in long-term deaths, cancer risk, cardiovascular disease, and diabetes.
“Physicians should counsel patients that bariatric surgery, like any surgical procedure, has some inherent risks,” he added. Mortality rates are currently less than 0.1% and major short- and long-term complication rates range from 1% to 4%.
Risks also vary depending on individual patient factors and the type of bariatric procedure, such as sleeve gastrectomy, Roux-en-Y gastric bypass, or the adjustable gastric band.
Whether the association with bariatric surgery was behind Presley’s death, “It’s so important to outline how safe bariatric surgery actually is. We get most people through surgery ‘healthy, hale and hearty,’” Kurian said.
Anti-Obesity Medications vs. Surgery?
Asked if the growing popularity of anti-obesity medications like Wegovy or off-label use of Ozempic will decrease weight loss surgery, Kurian was doubtful.
“Bariatric surgery, actually, I think will not drop off,” she said. “These drugs are helpful, but the ones that we currently have have not taken off as much weight as surgery.”
Kurian believes surgery offers a more durable approach to treating severe obesity.
Ultimately, a decision on anti-obesity medication and/or bariatric surgery should be individualized and based on a discussion between a patient and their doctor. It also depends, in part, on how much weight a person would need to lose to be healthier, Kurian said.
“These medications are a fantastic addition to our armamentarium for the treatment of obesity,” Brethauer said. “These injectable medications actually mimic the same gut hormone changes we see after metabolic procedures like gastric bypass, sleeve gastrectomy, and duodenal switch.
“Both bariatric surgery and pharmacological agents like the GLP-1 receptor agonists are safe and effective, and we use these medications before and after surgery to promote additional weight loss and control hunger,” Brethauer added. The biggest difference between the two approaches is changes from surgery are more permanent compared to the medications that require taking on an ongoing basis.
On the plus side, more people are talking about obesity with the popularity of Wegovy, Ozempic, and other anti-obesity medications. This could help remove some of stigma around obesity, Kurian said, and “it makes everyone realize that it’s not just about diet and exercise.”
“It’s wonderful that people are getting help understanding … that it’s not just their failure but that there are physiologic and hormonal reasons for the inability to lose weight easily.”