Kristamarie Collman, MD, had long had heavy menstrual periods. But 4 years ago, she started to notice other things that seemed off. She felt unusual pressure in her lower abdomen. She was going to the bathroom more often. The ab exercises that were part of her fitness routine had become harder to do. The combination of symptoms prompted Collman, who is a family doctor in Orlando, to see her doctor.
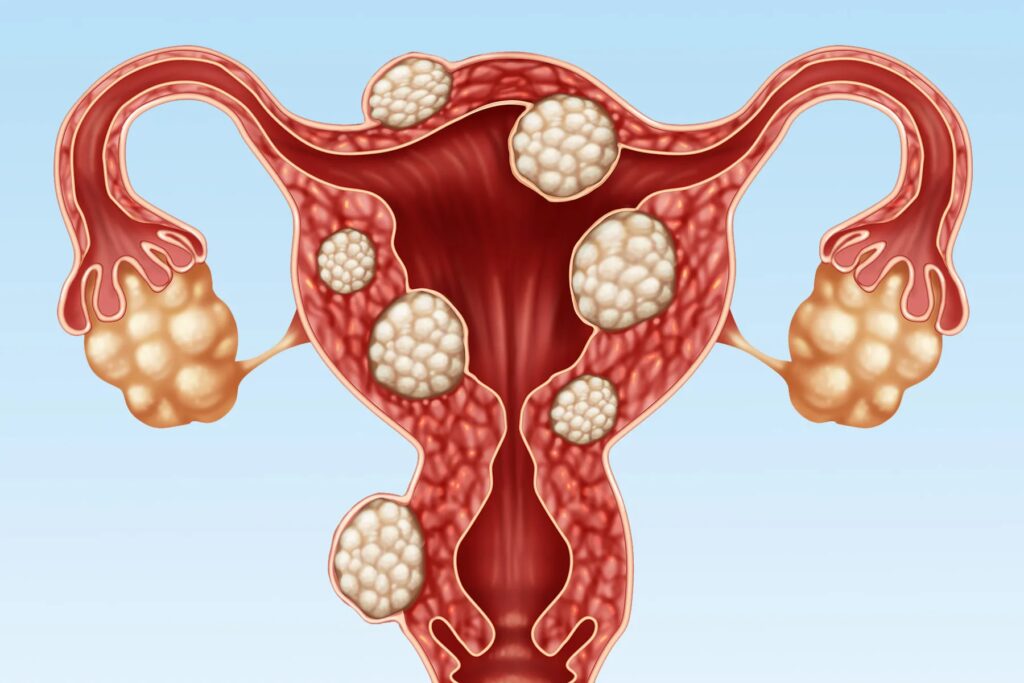
The diagnosis: uterine fibroids. These are tumors in the uterus that are almost always not cancer. Uterine fibroids are very common. Experts estimate that up to 80% of women develop them by age 50. No one knows exactly what causes them; a mix of factors are likely involved.
Some women have uterine fibroids and don’t know it because they have no symptoms. Others have a much harder time. Symptoms can include heavy bleeding, painful periods, pain during sex, reproductive problems, and other issues.
Collman had suspected that she might have fibroids. “But it’s not something that runs in my family,” she says. When she was diagnosed, “I was a little surprised but not completely shocked because we know Black women have a higher chance of getting diagnosed with fibroids,” Collman says.
Black women develop fibroid tumors 10 years earlier than white women do and are four to five times more likely to have one or more tumors, says Serdar Bulun, MD, the John J. Sciarra Professor of Obstetrics and Gynecology at Northwestern University.
The reasons for that aren’t clear. Even though uterine fibroids are very common, they aren’t studied enough, Bulun says.
Even though fibroids are almost never cancerous, “the symptoms can be really, really devastating although they are not malignant,” Bulun says. He directs the only National Institutes of Health-funded basic science research program focusing on fibroids in the U.S.
What’s Behind the Disparity?
It’s a question with no simple answer. Complex factors are involved in this common disease, says Erica Marsh, MD, professor of obstetrics and gynecology at the University of Michigan Medical School.
Genes and hormones likely play a role in who develops uterine fibroids. For instance, fibroids often stop growing or even shrink in menopause, when hormone levels are lower.
There are also some other general patterns: Fibroids are also more likely if they run in your family, you’re overweight, or you eat a lot of red meat or ham, according to the U.S. Department of Health & Human Services Office on Women’s Health. And some research shows that women diagnosed with uterine fibroids are more likely to have depression and anxiety than women without fibroids. It’s not clear why that is or which comes first.
The disparity in uterine fibroids may be partly influenced by the following things, according to Marsh and Bulun:
Chronic stress. This is stress that lasts a long time. It’s long been linked with many health conditions. And it can include stress from racism. “We know that one of the most significant forms of chronic stress that Black individuals experience is that of racism,” Marsh says.
Marsh and colleagues reviewed studies of racial disparities in who gets fibroids and another condition, endometriosis. Their findings, published in the journal Fertility and Sterility in March 2023, show a link between certain life experiences, including exposure to racism, and fibroids in Black women.
It’s not possible to prove that racism causes fibroids. But “there’s at least evidence, epidemiologic or preliminary data, that says there is an association between exposure to racism and increased risk of fibroids,” Marsh says.
In a separate study, Bulun and his team analyzed uterine fibroid tissues from white American, Black American, and Japanese patients. The biggest differences were between the fibroids of Black American women and Japanese women. “We found that Black patients’ fibroids had increased estrogen formation and they were making more estrogen, and that’s also contributing to fibroid growth,” he says.
Bulun says that genes and ancestry play a role in this and that it’s “totally plausible that chronic stress can increase estrogen production in the body.”
Exposure to phthalates. Phthalates are chemicals found in a wide variety of products, including chemical hair straighteners. Bulun’s team analyzed levels of a particular phthalate in 712 uterine fibroid patients. They found a strong link between that phthalate and uterine fibroids. Their study, published in the Proceedings of the National Academy of Sciences in November 2022, didn’t trace the source of the phthalates in the women and doesn’t prove that those chemicals cause fibroids. But Bulun and colleagues had previously reported a possible link between chemical hair straighteners and uterine fibroids. “We believe that phthalates are more commonly present in hair straighteners,” Bulun says. “These products are more commonly used by Black women versus other populations.”
MED12 genetic mutation. Finnish researchers found that some 70% of fibroid tumors are linked to a genetic mutation called MED12. Bulun says that this mutation happens during the second half of a woman’s menstrual cycle when cells in the myometrium, or smooth muscle of the uterus, multiply in preparation for pregnancy.
The Finnish study didn’t specify the racial or ethnic background of the women whose fibroids were studied. “It’s possible that Black women of sub-Saharan ancestry might be more prone to genetic alterations or mutation formation in that MED12 gene for reasons we don’t understand,” Bulun says. He notes that it’s also possible that chronic stress could stimulate the tumors to grow big enough for doctors to find them. More research is needed to learn whether this is happening and how it unfolds.
Having lived with fibroids herself, Collman has this advice for women: “I would advise anyone reading this story to not wait, not second-guess themselves. If they don’t feel like something’s right, they notice a change, they notice certain symptoms, then I would encourage them to seek help, whether it’s with their doctor [or] health care team. They should not dismiss their symptoms.”