March 30, 2023 — A federal judge in Texas on Thursday struck down the preventive services mandate of the Affordable Care Act, ruling that the need to provide these services violated the religious rights of the plaintiffs.
One of the plaintiffs who filed the lawsuit is Steven Hotze, MD, a Texas doctor and conservative talk radio host. He said providing health insurance coverage for medication taken daily to prevent HIV to his employees would make him complicit in behaviors that he said violate his religious beliefs.
The ruling applies nationwide, and public health experts were quick to criticize the decision.
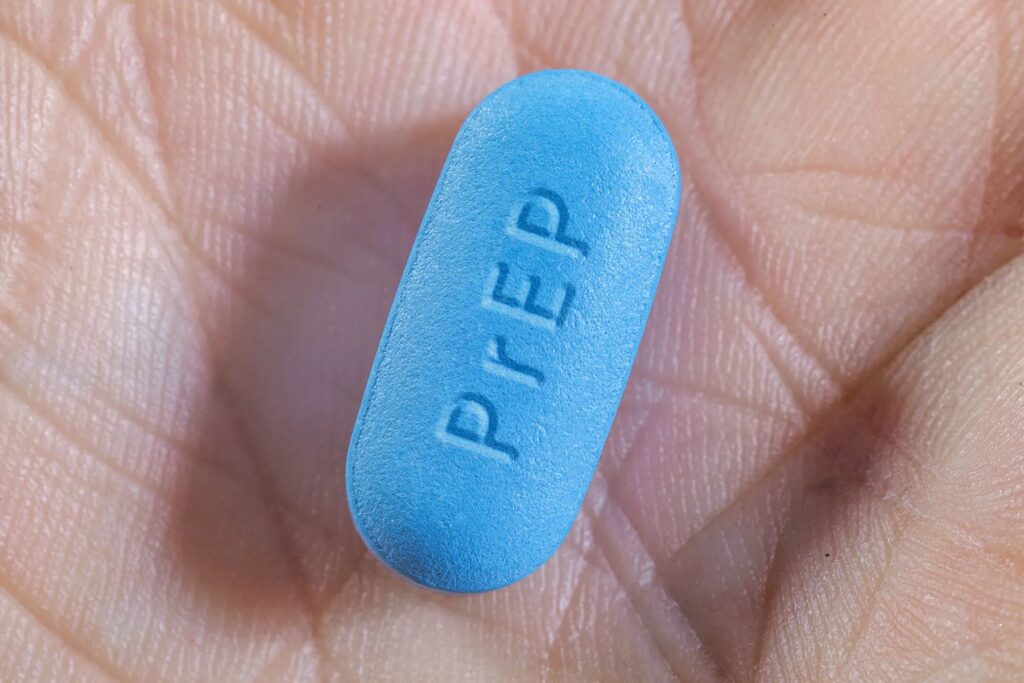
“The human cost of this decision is very real,” said Meredithe McNamara, MD, an assistant professor of pediatrics and adolescent medicine specialist at Yale University. Yale researchers, anticipating the ruling, estimated in a recent study that eliminating coverage of the medication, known as PrEP (preexposure prophylaxis), which was mandated for health insurers under the Affordable Care Act, will result in at least 2,000 new HIV infections within a year.
The two brand-name medications approved for PrEP, Truvada and Descovy, cost about $1,800 a month or more without insurance. Generic versions are available for less but are not always available, experts said. Other financial programs, including some by drugmakers, offer assistance to those who qualify. The mandate to provide PrEP coverage began in June 2020, after the U.S. Preventive Services Task Force (USPSTF), an independent panel of experts, gave it an “A” recommendation. Federal law requires any preventive services with an A or B to be covered.
The ruling could also affect much more than just insurance coverage of PrEP. American Medical Association President Jack Resneck Jr., MD, in a statement, said the ACA required insurers and health plans to cover dozens of preventive health services with no cost to patients for things like early detection of cancer, hypertension, diabetes, and sexually transmitted infections.
“Millions of patients could lose first-dollar coverage for cholesterol treatment, tobacco and alcohol cessation, immunizations, and childhood screenings for lead poisoning, hearing loss, and autism,” he said. “Care that is critical to reducing maternal mortality would also be jeopardized. These preventive-care requirements that for 10 years have enabled millions of Americans to improve their health could just go away as a result of this flawed ruling.”
“The government will surely appeal, and has every right to do so,” said Nicholas Bagley, a professor of law at the University of Michigan. “The big question is whether the courts will enter a stay, pending the appeal. I’d expect them to do so, but we will see.”
Even without a stay, Bagley said, most insurance plans are annual, so coverage may not change right away, but that’s not certain. The ruling applies to preventive care guidelines issued after 2010, when the Affordable Care Act was enacted. The contraceptive mandate has been challenged in this case, Bagley said, but was rejected in September. He expects that decision to be appealed.
HIV Prevention: Key Strategy
Prevention, including the use of PrEP, is a key strategy of the federal initiative Ending the HIV Epidemic in the U.S. It aims to decrease new diagnoses to 3,000 by 2030. New diagnoses had decreased 8% from 2016 to 2019, according to the CDC, but there is work to be done to reach the 2030 goal. In 2020, there were 30,635 new HIV diagnoses. When taken correctly, PrEP reduces the risk of becoming infected by 99%, according to the CDC.
In 2020, about 25% of the 1.2 million people in the U.S. for whom PrEP was recommended were actually prescribed it, up from about 3% in 2015, according to the CDC.
One of those is Dan, a gay marketing professional in the Midwest who asked that his real name not be used. He has taken PrEP for about a decade. His employer’s health insurance plan covers it, and it’s important to him.
“I am sexually active, but not that much,” he said. Even so, he counts on the medication for protection when he is sexually active. If the coverage is taken away? “I would probably stop taking it,” he said.
Yale Study and the Effect of Ending the Coverage
Researchers from Yale University estimate that eliminating the PrEP coverage would result in at least 2,000 entirely preventable HIV infections in the following year, as PrEP usage declines without the mandated coverage. That estimate only takes into account the effect on men who have sex with men, not other people also at risk for HIV infection who could benefit from PrEP, such as those who inject drugs or women who have sex with an infected person.
As a result, the estimate is very conservative, says study leader A. David Paltiel, PhD, a professor of health policy at the Yale School of Public Health. His team used U.S.-based data on HIV infection, current rates of PrEP coverage and effectiveness, and the estimated reduction in coverage if access to private health insurance benefits were curtailed.
“We underestimated the number knocked out of PrEP coverage” if the repeal goes national, he said. Right now, about 28% of all men who have sex with men are getting coverage for PrEP, Paltiel estimates. “For every 1% drop from the 28%, there would be 114 new infections,” he said. The researchers also calculated that the percentage of people taking the drug would drop to about 10%. “If that happened, it will result in about 2,000 new infections in the following year. OK? There are people who are going to be left high and dry.”
More on Braidwood Management v. Becerra
In the lawsuit, Braidwood Management v. Becerra, several Christian-owned businesses and several people in Texas sued the federal government, saying the preventive services mandate violates their religious beliefs under the Religious Freedom Restoration Act, a 1993 federal law that guarantees interests in religious freedom are protected.
The plaintiffs also argue that the Affordable Care Act requirement to provide recommended preventive services violates the Constitution’s Appointments Clause, which requires people the president appoints to positions be confirmed by the Senate. The Preventive Services Task Force members are instead appointed by the heads of agencies within the Health and Human Services Department.
Since it was created in 1984, the task force has weighed in on numerous preventive measures, such as when to screen people for diseases and other questions, making evidence-based recommendations to help health care providers care for patients.
More Reactions
In a statement, Bruce J. Packett, executive director of the American Academy of HIV Medicine, said the Yale report “highlights the critical necessity of taking into account public health repercussions of judicial decisions.”
The effects of eliminating coverage could be catastrophic for HIV reduction efforts, he said. And, he pointed out, “the report only accounts for the effects of not requiring insurers to cover PrEP through one year; the authors did not calculate primary HIV transmissions that would happen well after a year and the secondary infections from those primary infections.”
Also at risk, Packett said, is the authority of the Preventive Services Task Force.
“Striking down the USPSTF’s ability to recommend important evidence-based health care preventive services would be detrimental across the entirety of the public health goals of the United States,” he said.
The Braidwood Management case is “misreading science,” according to McNamara and other Yale researchers. In mid-February, they posted a report, explaining how the PrEP mandate promotes public health not for a segment of the population but the population as a whole. PrEP benefits public health, much like any vaccine or other preventive measure for avoiding infection.
The researchers call PrEP “one of the most celebrated biomedical successes in the global fight to end the HIV epidemic.”
The harms of granting a nationwide injunction against requiring health insurance plans to cover PrEP would affect some ethnic groups disproportionately, McNamara said. Most affected, she said, would be Black and Latino gay and bisexual men, as well as transgender women.
Younger at-risk people would also be at a disadvantage, said McNamara, who cares for adolescents in her clinic. “I can tell you that not having cost sharing for HIV prevention essentially means they aren’t going to use it at all,” she said.