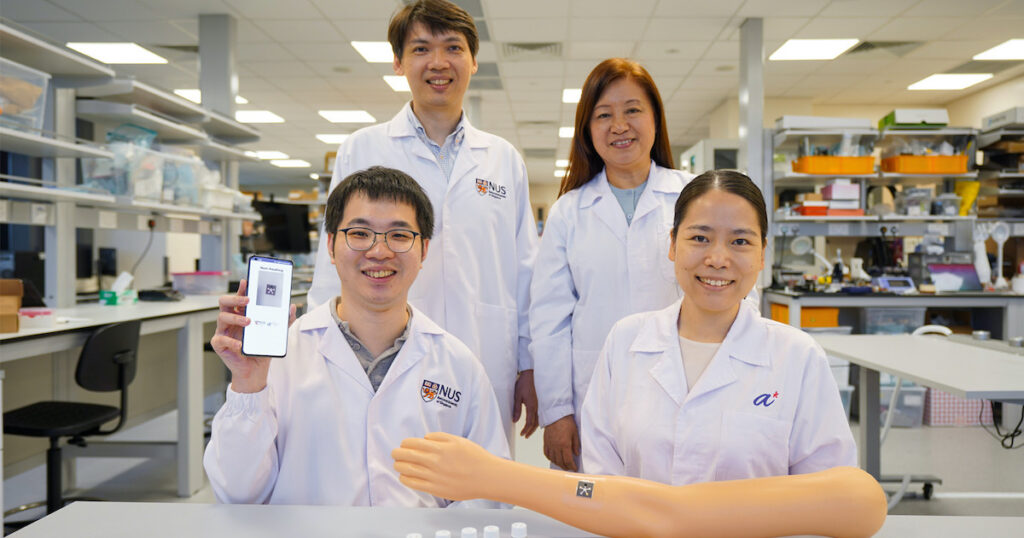
Researchers from the National University of Singapore and A*STAR’s Institute of Materials Research and Engineering have developed an AI-powered sensor patch for monitoring wound recovery.
WHAT IT DOES
Called PETAL (Paper-like Battery-free In situ AI-enabled Multiplexed), the patch comprises five colourimetric sensors in a fluidic panel patterned after a five-petal pinwheel flower. Each of the petals acts as a sensing region that detects and measures wound biomarkers, namely: temperature, pH, trimethylamine, uric acid and moisture, within 15 minutes.
Without removing the sensor from the wound, an image or video of the sensor patch can be recorded on a mobile phone for analysis and classification using a proprietary AI algorithm.
Findings from a study published in the journal Science Advances showed PETAL to achieve 97% accuracy in differentiating healing and non-healing chronic and burn wounds.
WHY IT MATTERS
Monitoring the status of wound recovery is crucial to wound care and management. Impaired wound healing, such as chronic wounds and post-burn pathological scars, could lead to life-threatening complications and further economic burden to patients and the healthcare system.
Doctors are still visually inspecting wound recovery by manually removing wound dressing, which can both be time-consuming and raise the risks of infection.
The research team from NUS and A*STAR combined their expertise in flexible electronics, AI, sensor data processing and nanosensor capabilities to come up with a solution that can be used for “prompt, low-cost wound care management” at hospitals and even at home.
While there are already existing wearable wound sensors, these can only measure one or a small number of parameters, as well as require bulky printed circuit boards and batteries. Meanwhile, PETAL was designed to be thin, flexible, and biocompatible so it can be easily and safely integrated with wound dressing, according to Dr Su Xiaodi, principal scientist of the Soft Materials Department at A*STAR IMRE.
NUS noted that their AI-enabled sensor can be adapted and customised for other wound types by incorporating other colourimetric sensors, such as glucose, lactate, or Interleukin-6 for diabetic ulcers. More detection zones can also be added to detect other biomarkers.
The research team has already filed an international patent for their invention; they are also planning to get the sensor into human clinical trials soon.
THE LARGER TREND
Previously, a research team from the NUS Department of Biomedical Engineering and the Institute for Health Innovation and Technology invented a similar technology for assessing chronic wounds wirelessly and in real time. The smart bandage called VeCare uses an electrochemical system to detect temperature, acidity, bacteria type and inflammatory factors specific to chronic wounds within 15 minutes. But unlike PETAL, VeCare is powered by a rechargeable battery.